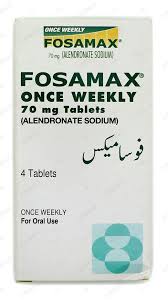
Fosamax
Fosamax, the esteemed brand name for alendronate sodium, is a distinguished medication primarily employed in the treatment and prevention of osteoporosis—a condition marked by fragile bones that are susceptible to fractures—as well as other bone disorders such as Paget’s disease. This pharmaceutical marvel belongs to the bisphosphonate class of drugs, which are designed to influence…